AAHomecare Ranks Medicare Reimbursement Priorities
Association outlines how HME industry can capitalize on an ‘unprecedented opportunity’ to obtain meaningful reimbursement adjustments.
The American Association for Homecare reports it has been closely coordinating with key legislators and committee staff to set the stage for an advocacy campaign for more sustainable Medicare reimbursement rates in former CBAs and other areas.
While CMS decided not to issue contracts for 13 categories of Round 2021 and has relaxed a number of regulations in order to help the industry continue providing service to Medicare patients during COVID-19, reimbursement rates have not seen a significant adjustment in six years. Furthermore, DEMPOS reimbursement rates don’t reflect the modern-day cost structure of serving patients, meaning that those reimbursement rates amount to less, the association emphasized in a public statement.
The problem is only compounded by state Medicaid programs, private payer insurance, and other funding sources that tie their reimbursement to Medicare rates.
To address this long-standing problem, AAHomecare is working has proposed a number of legislative and regulatory priorities on Capitol Hill it intends to pursue on Capitol hill:
- Implement a 90/10 blended rate for former CB areas. Using a similar methodology to the 50/50 blended rates for rural areas and 75/25 blended rates for other non-CB areas currently in effect, AAHomecare is recommending that former CBAs receive 90 percent adjusted and 10% unadjusted rates (90/10 Blended Rates). This approach will provide an average of 15% increase for the top HCPCS code of each product category and is consistent with rate relief policies in rural and non-rural areas.
- Apply the 90/10 Blended Rates to all items formerly covered under the bidding program. The average impact of a 90/10 blended rate for the 94 top HCPCS codes across 13 categories can be found here. A selection of examples from that list are shown with additional detail in the figure below. AAHomecare noted that the figures do not take into account the April 2021 increases for oxygen stemming from the budget neutrality fix, so actual oxygen rates will be slightly higher.
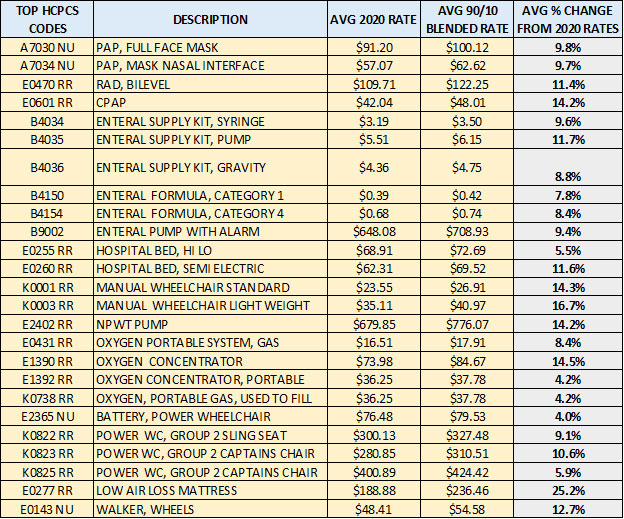
Image Source: AAHomecare
- Formally adopt rural and non-bid area rates. AAHomecare will also seek permanent adoption of currently-in-effect 50/50 blended rates for rural suppliers and 75/25 blended rates for non-rural, non-CBA suppliers.
“CMS delayed a new round of bidding for two years and then subsequently scrapped most of the bidding program because bids based on the product costs and market conditions faced by HME suppliers didn’t result in further rate reductions,” said Tom Ryan, AAHomecare president and CEO. “It was clear that the HME sector was due for significant rate adjustments even before the COVID-19 pandemic hit. Now product and operational costs are even higher and the need for market-based rates is even more evident.”
Ryan stressed that a substantial adjustment is needed because, in addition to marketplace realities, HME providers cannot pass rising costs on to patients given that they are under fixed fee schedules.
“Given the failure of the last bidding round and the need to strengthen our nation’s ability to provide cost-effective care to seniors and other individuals at home, now is the time to get HME reimbursement policy right,” Ryan said. “We have an opportunity to establish reimbursement rates that will allow HME suppliers to play a major role in supporting America’s fast-growing cohort of seniors and helping them stay close to their families and communities. We have to take advantage of this chance to secure a long-term, sustainable rates for HME.”